Bottled and Well Water Quality in a Small Central Appalachian Community: Household-Level Analysis of Enteric Pathogens, Inorganic Chemicals, and Health Outcomes in Rural Southwest Virginia
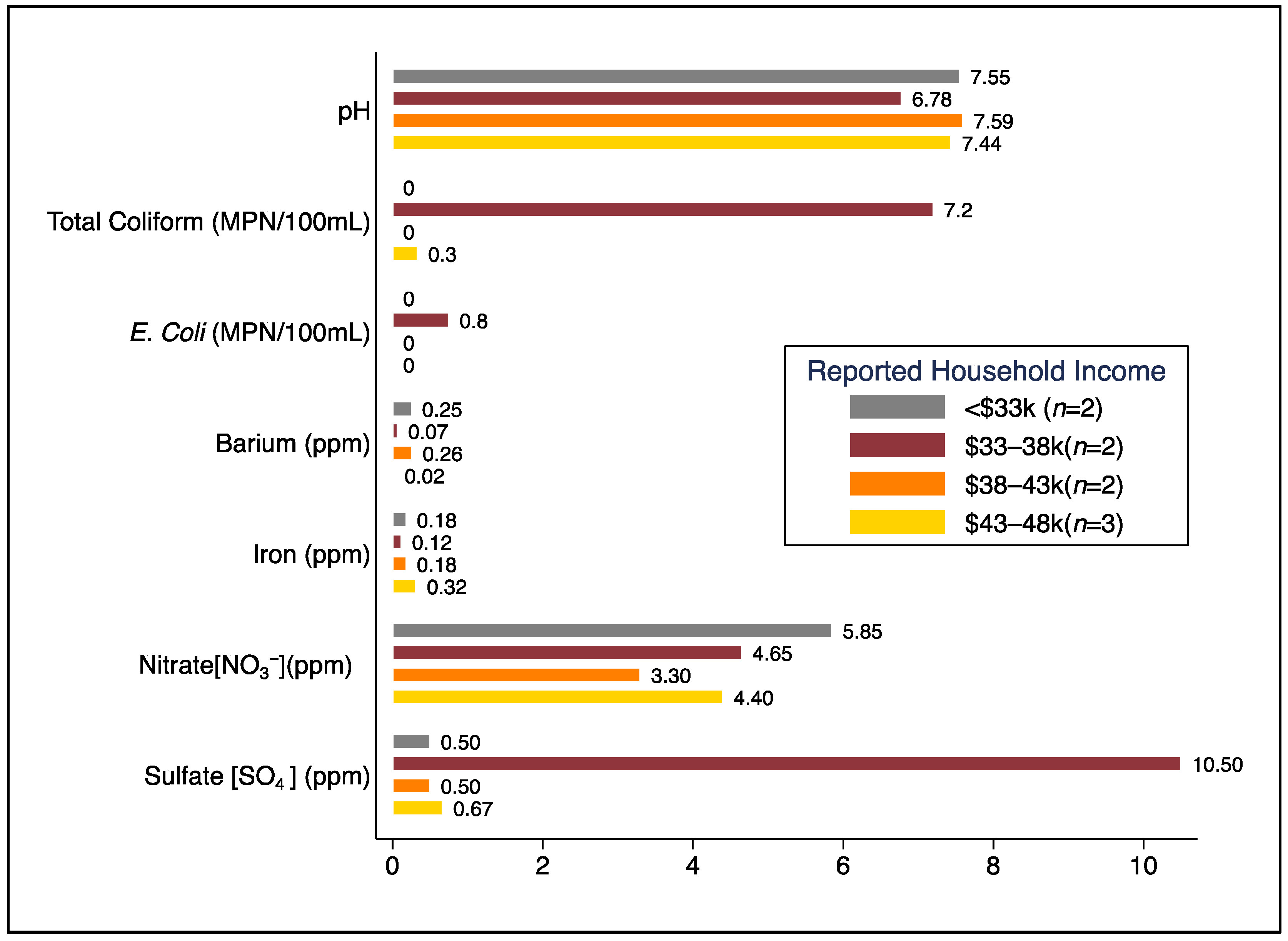
Abstract/Summary: Consumption of unsafe drinking water is associated with a substantial burden of disease globally. In the US, ~1.8 million people in rural areas lack reliable access to safe drinking water. Our objective was to characterize and assess household-level water sources, water quality, and associated health outcomes in Central Appalachia. We collected survey data and water samples (tap, source, and bottled water) from consenting households in a small rural community without utility-supplied water in southwest Virginia. Water samples were analyzed for physicochemical parameters, total coliforms, E. coli, nitrate, sulfate, metals (e.g., arsenic, cadmium, lead), and 30+ enteric pathogens. Among the 69% (n = 9) of households that participated, all had piped well water, though 67% (n = 6) used bottled water as their primary drinking water source. Total coliforms were detected in water samples from 44.4% (n = 4) of homes, E. coli in one home, and enteric pathogens (Aeromonas, Campylobacter, Enterobacter) in 33% (n = 3) of homes. Tap water samples from 11% (n = 1) of homes exceeded the EPA MCL for nitrate, and 33% (n = 3) exceeded the EPA SMCL for iron. Among the 19 individuals residing in study households, reported diarrhea was 25% more likely in homes with measured E. coli and/or specific pathogens (risk ratio = 1.25, cluster-robust standard error = 1.64, p = 0.865). Although our sample size was small, our findings suggest that a considerable number of lower-income residents without utility-supplied water in rural areas of southwest Virginia may be exposed to microbiological and/or chemical contaminants in their water, and many, if not most, rely on bottled water as their primary source of drinking water.
Bottled and Well Water Quality in a Small Central Appalachian Community: Household-Level Analysis of Enteric Pathogens, Inorganic Chemicals, and Health Outcomes in Rural Southwest Virginia
Authors: Cohen, A., Rasheduzzaman, M., Darling, A., Krometis, L.-A., Edwards, M., Brown, T., Ahmed, T., Wettstone, E., Pholwat, S., Taniuchi, M., & Rogawski McQuade, E. T.
Publication Year: 2022 | Journal / Publisher: International Journal of Environmental Research & Public Health
Abstract/Summary: Consumption of unsafe drinking water is associated with a substantial burden of disease globally. In the US, ~1.8 million people in rural areas lack reliable access to safe drinking water. Our objective was to characterize and assess household-level water sources, water quality, and associated health outcomes in Central Appalachia. We collected survey data and water samples (tap, source, and bottled water) from consenting households in a small rural community without utility-supplied water in southwest Virginia. Water samples were analyzed for physicochemical parameters, total coliforms, E. coli, nitrate, sulfate, metals (e.g., arsenic, cadmium, lead), and 30+ enteric pathogens. Among the 69% (n = 9) of households that participated, all had piped well water, though 67% (n = 6) used bottled water as their primary drinking water source. Total coliforms were detected in water samples from 44.4% (n = 4) of homes, E. coli in one home, and enteric pathogens (Aeromonas, Campylobacter, Enterobacter) in 33% (n = 3) of homes. Tap water samples from 11% (n = 1) of homes exceeded the EPA MCL for nitrate, and 33% (n = 3) exceeded the EPA SMCL for iron. Among the 19 individuals residing in study households, reported diarrhea was 25% more likely in homes with measured E. coli and/or specific pathogens (risk ratio = 1.25, cluster-robust standard error = 1.64, p = 0.865). Although our sample size was small, our findings suggest that a considerable number of lower-income residents without utility-supplied water in rural areas of southwest Virginia may be exposed to microbiological and/or chemical contaminants in their water, and many, if not most, rely on bottled water as their primary source of drinking water.
PDF on Publisher Website | PDF on OSF